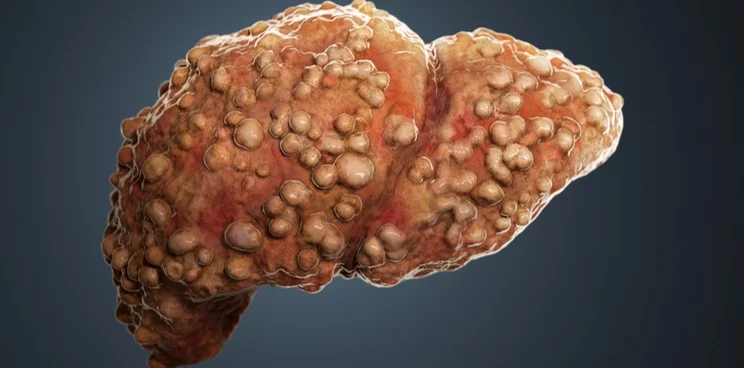
What is Cirrhosis?
Cirrhosis is a chronic, progressive liver disease marked by the replacement of normal liver tissue with scar tissue. This scarring disrupts the liver’s normal functioning, impairing its ability to process nutrients, hormones, drugs, and toxins, as well as produce proteins and other substances vital for health.

What Causes Cirrhosis?
Common causes include excessive alcohol consumption (alcoholic cirrhosis), chronic hepatitis (especially hepatitis B and C), and non-alcoholic fatty liver diseases (NAFLD and NASH). Other risk factors include inherited diseases like hemochromatosis and autoimmune liver diseases.
What are Its Most Common Symptoms?
Symptoms may not be apparent in its early stages. As the disease progresses, symptoms such as fatigue, loss of appetite, weight loss, nausea, weakness, and mental confusion can arise. In more advanced stages, jaundice (yellowing of the skin and eyes), fluid accumulation in the abdomen (ascites), and a tendency to bleed or bruise easily may appear.
Early detection of cirrhosis is challenging due to the lack of apparent symptoms. Regular medical examinations are crucial, especially for those with risk factors such as excessive alcohol consumption or pre-existing liver disease.
What Modern Treatments are Applied to Patients?
While there is no cure for cirrhosis, its progression can be slowed or halted by treating the underlying cause. Treatment might include abstaining from alcohol, medication to control hepatitis or fatty liver disease, and lifestyle changes like a healthy diet and exercise. Advanced treatments include antiviral drugs for hepatitis, therapies for portal hypertension, and, in severe cases, liver transplantation.
This complex procedure involves replacing the damaged liver with a healthy one from a donor, offering a chance for improved health. Regular monitoring and an interdisciplinary approach are pivotal for comprehensive cirrhosis management.